Other associated problems
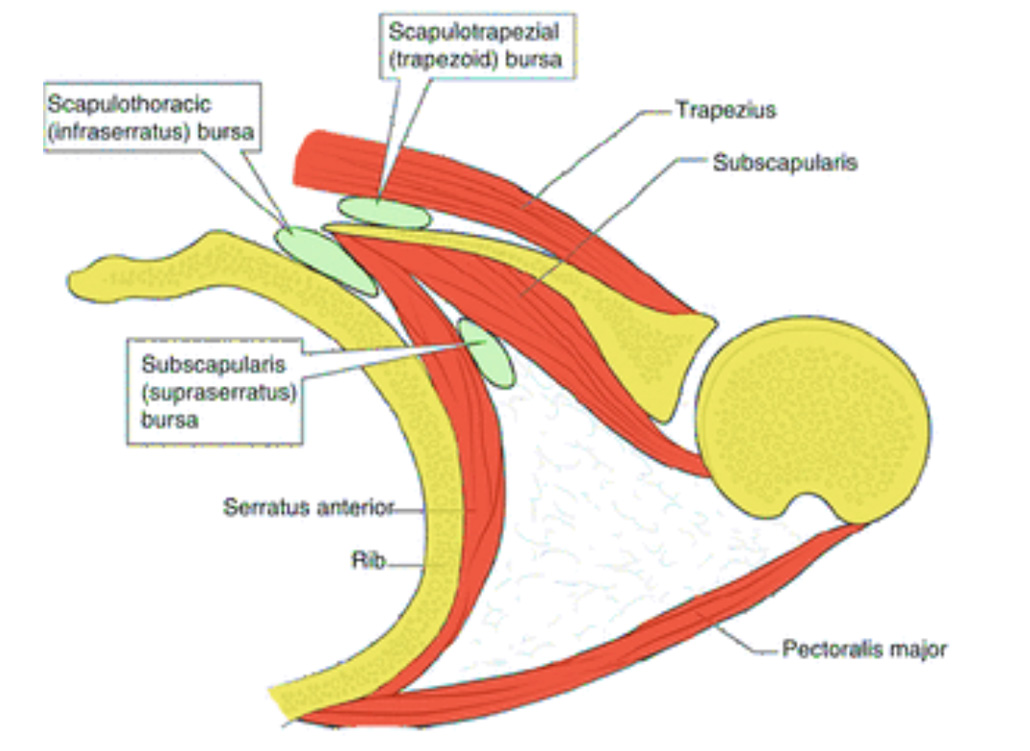
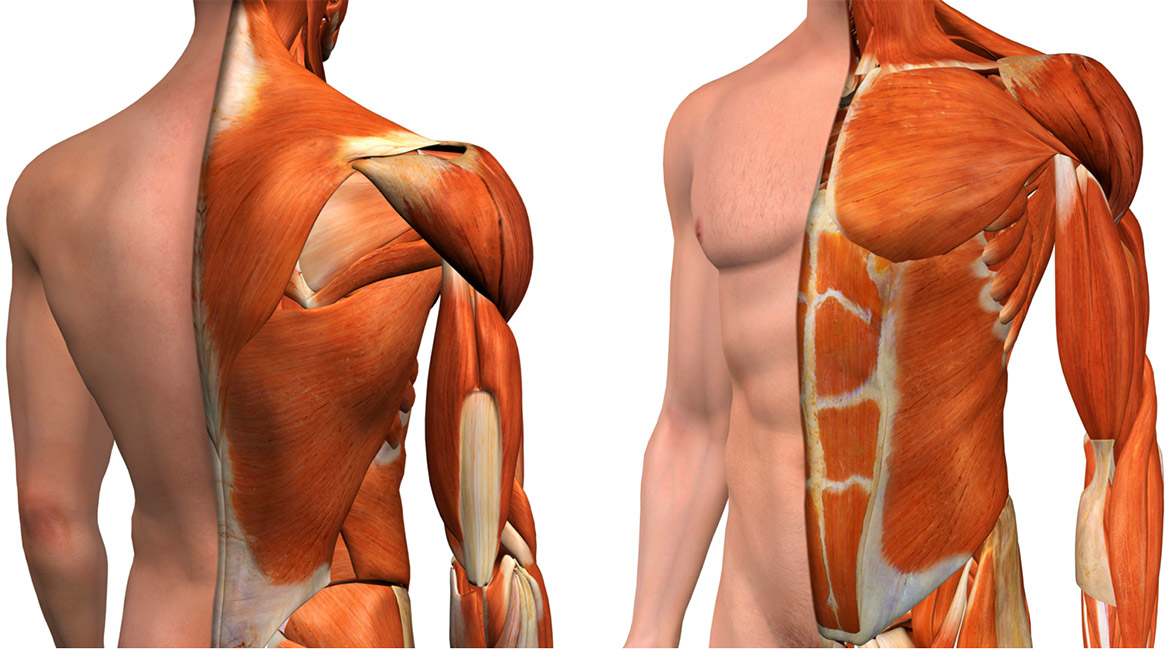
Other common sites of injury or problems include the clavicle (collar bone) and scapula (shoulder blade), and together with the upper arm (humerus) are known as the shoulder or pectoral girdle. With the muscles covering these three bones the shoulder joint is stabilised and allows the shoulder girdle to move the arm in multiple directions. The relationship between the clavicle and the sternum – the Sternoclavicular joint; and the scapula and underlying ribs - Scapulothoracic joint are important areas that can cause pain, swelling and dysfunction (problems with movement) that may present with a chest wall problem. In addition, the thoracic part of the vertebrae (back bone) and its rib junction are another common source of pain and chest wall problems.
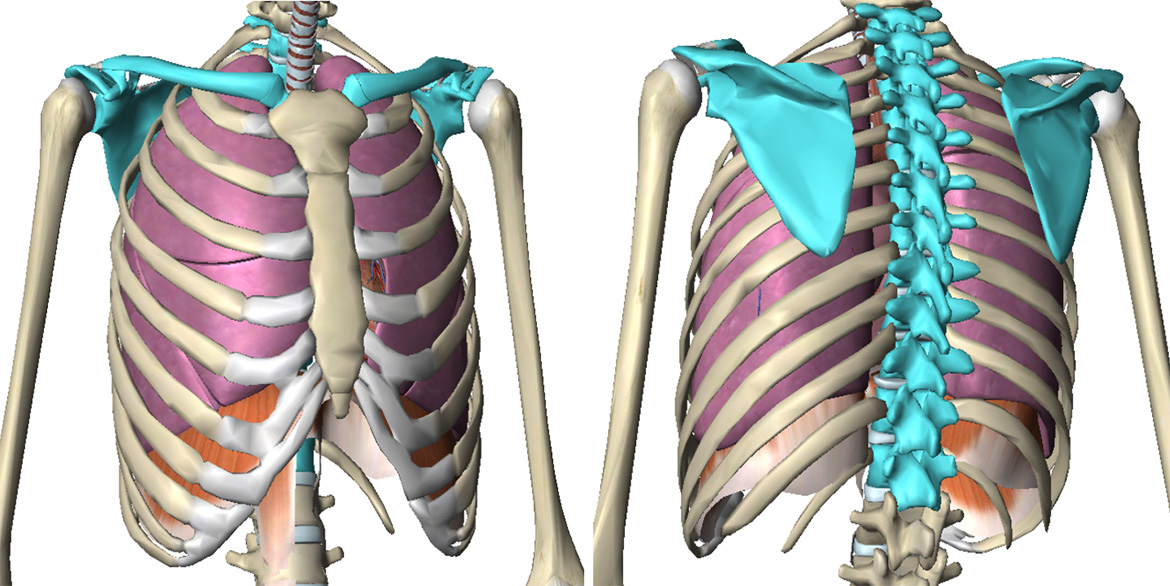
Illustration of the shoulder girdle (clavicle & scapula) and thoracic spine (in blue)
Sternoclavicular Joint
The joint between the sternum (specifically the manubrium) and the clavicle. It is the only joint that links the bones of the shoulder (and arm) to the axial skeleton (chest and spine bones). Tough bands of connective tissue called ligaments surround the Sternoclavicular (SC) joint, gives it strength and stability. It is important because it helps support the shoulder.
CT reconstruction of sternoclavicular joint (in red)
Symptoms
The most common symptom of an SC joint problem is pain. The type of pain and severity depends on the underlying problem, if traumatic and acute but minor the pain may feel like a bruise with no other associated features, if severe as in a fracture or dislocation the pain can be severe, especially when you attempt to move your arm. Other features may include: Swelling, bruising, or tenderness over the joint. A crunching or grinding sound when you try to move your arm and a limited range of motion in the arm.
With non-traumatic problems as in inflammatory conditions, such as rheumatoid arthritis, pain be felt in other joints and is more chronic. With a joint infection, there may be redness over the joint and you may have fever, chills, or night sweats.
Dislocation of the SC joint. Following trauma, the SC joint can dislocate forwards over the sternum (anterior dislocation) or backwards behind the sternum (posterior dislocation). Occasionally, particularly in young people a part of the clavicle next to the sternum called the physis (or growth plate) can fracture as its still soft in people under 25.
Anterior SC joint dislocation is more common and is typically associated with a lump over SC joint. They can often be managed without the need for surgical correction. The posterior SC joint dislocation is rarer but potentially more serious as it can push or even injure structures behind the sternum including blood vessels, the windpipe or oesophagus. Surgery to correct may be necessary.
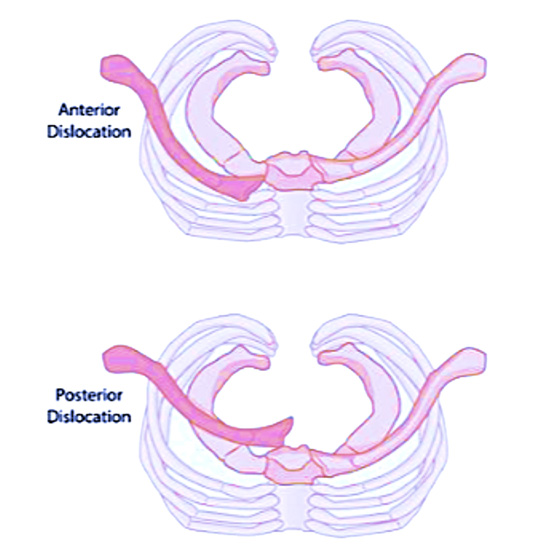
Anterior and posterior dislocation of the SC joint
As well as SC joint dislocations and even fractures through the clavicular growth plate (distal clavicle physeal fractures), simple sprain of the SC joint can occur without joint instability and rarely ligament injuries can lead to a stable but painful joint that clicks, grates or pops. A more unusual condition, Spontaneous atraumatic subluxation of the sternoclavicular joint can occur. The typical patient is a female with multidirectional instability and ligamentous laxity. There is an excessive but incomplete translation or rotation of the medial clavicle away from the sternum. This is often referred to as a sprain.
Non-traumatic inflammatory conditions of the SC joint, include forms of arthritis such as osteoarthritis, a type of degenerative arthritis that tends to get worse with age. Other types of inflammatory arthritis such as rheumatoid arthritis, typically affecting a younger population can cause pain and swelling of the SC joint.
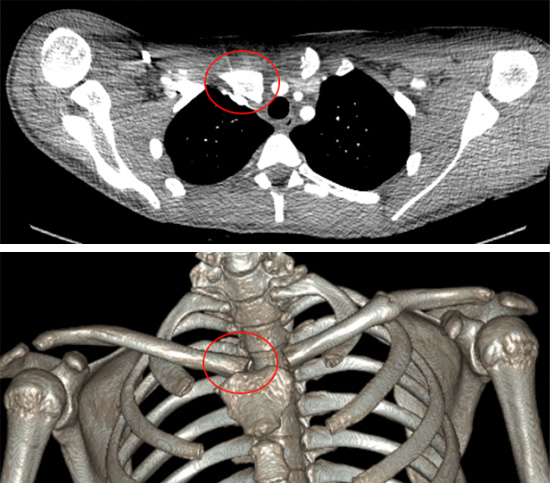
Chest CT with reconstructions showing an acute posterior SC joint dislocation (red ring) in a young rugby player
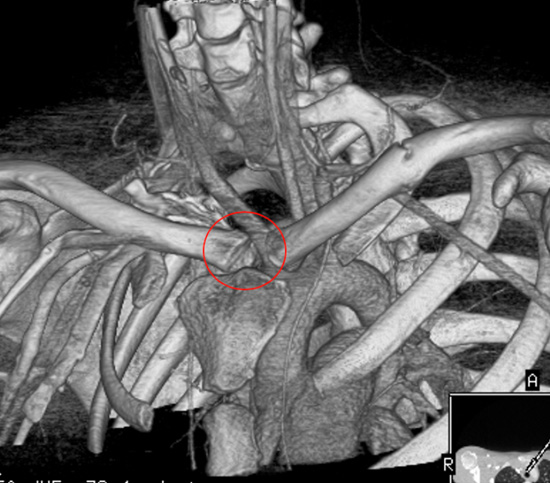
Septic arthritis of the sternoclavicular joint is an unusual infective condition, especially in otherwise healthy adults. Because it is associated with serious complications such as chest wall abscess and osteomyelitis (bone infection) prompt diagnosis and appropriate treatment are required.
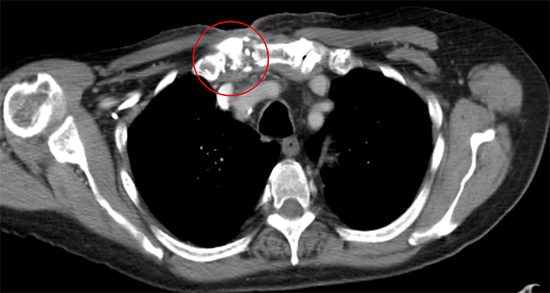
Chest CT showing right sided septic arthritis leading to osteomyelitis of the SC joint (red ring)
Other unusual often described as atypical conditions affecting the SC joint include Sterno- costoclavicular hyperostosis (SCCH) a chronic inflammatory disorder which presents with erythema, swelling, and pain of the sternoclavicular joint. Approximately one half of patients have acne or pustular lesions with the best described association being with palmoplantar pustulosis (PPP). Tietze’s syndrome can rarely affect the SC joint. See chest wall pain.
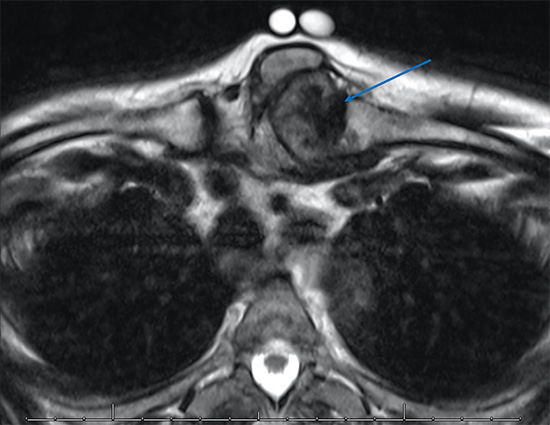
Chest MRI of a rare cause of a SC joint pain and swelling associated with a form of inflammatory or rheumatic arthritis, tophaceous gout (blue arrow). The swelling along with of part of the left SC joint and clavicle were removed surgically.
Scapulothoracic joint
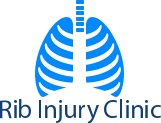
Unlike the SC joint this is not a true joint but rather an articulation between the anterior (front) surface of the scapula and posterior and lateral chest wall. For it to function it relies of the integrity of SC joint and the acromioclavicular (AC) joint where the end of the clavicle joins the scapula and the ‘scapulothoracic muscles’ that provide mobility and stability of scapula during shoulder girdle movements (essentially moving the upper arm).
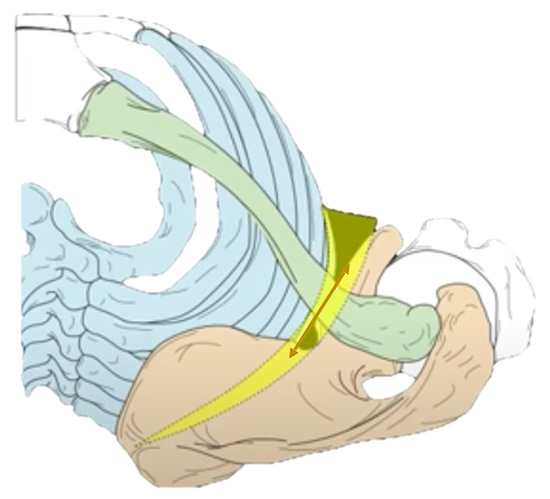
Scapulothoracic joint (yellow) and movement of the scapula (light brown) and clavicle (green) over the rib cage (blue)
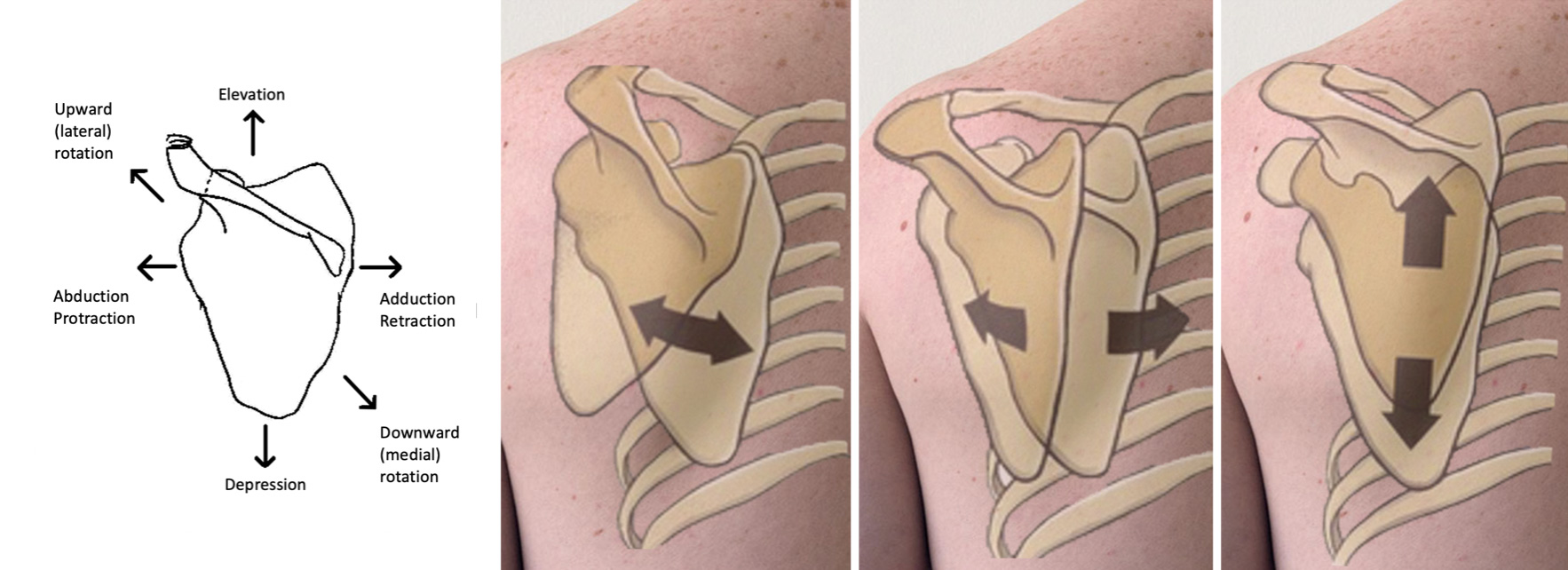
Scapulothoracic movements of the shoulder girdle
Symptoms
Often referred to a scapulothoracic dysfunction or dyskinesis, it refers to abnormal motion of the scapula during shoulder movement. The causes are multiple and include problems with any other one of more the components of the scapulothoracic joint including weakness, imbalance, tightness or detachment of one or more of the scapulothoracic muscles that control the scapula particularly the larger scapular muscles such as the serratus anterior, latissimus dorsi, rhomboids, and trapezius muscles. This may result from a nerve injury to one of these muscles. Another common cause is Injuries to the bones that support the scapula or injuries within the shoulder joint. These include injuries to the ribs that the scapula glides over leading to pain or if the ribs are significantly displaced impingement of scapula movement. Other injuries including to the scapula directly, to the clavicle and to the SC or AC joints can all lead to scapulothoracic dyskinesis.
Specific problems include winging of the scapula where the affected scapula appears to protrude particularly when leaning against an outstretched arm. This can be described clinically as partial or total winging and can be caused by muscle problems particularly to serratus anterior or an injury to the nerve supplying the muscle.

Postural asymmetry of scapula with winging of the scapula is typically considered to be associated with injuries. However, asymmetry in the overhead athlete's scapula may be normal due to the dominant use of the limb.
Another problem described is snapping scapula syndrome also known as scapulothoracic syndrome. It can be a form of scapulothoracic dyskinesis and seen in young, active patients who tend to excessively use the overhead or throwing motion. Another cause is when the muscles underneath the scapula (the subscapularis muscle) atrophies. This causes the scapula to become very close to the rib cage, eventually causing rubbing or bumping during arm/shoulder movement. Another cause is bursitis, which is when the tissues between the shoulder blade and thoracic wall (bursa) become inflamed. These bursae are small fluid-filled sacs designed to reduce friction between muscle or tendon and bone. These layers (superficial, intermediate, and deep) form a smooth surface for the scapula to move, glide, and rotate over. Muscle and bone abnormalities in the shoulder area can also contribute to the pain.
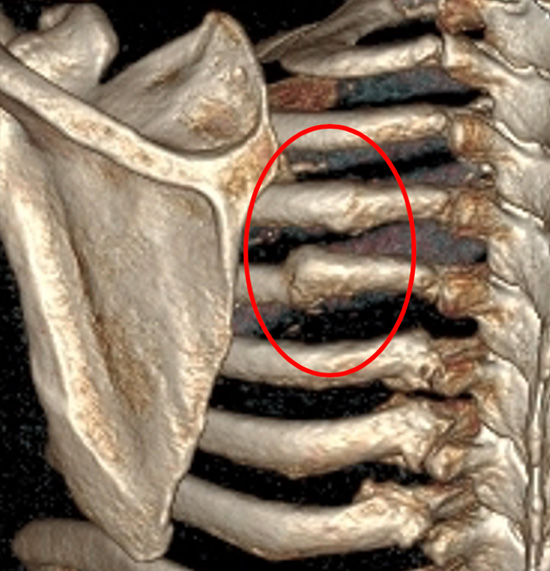
Chest CT reconstruction showing old poorly healed rib fractures (red ring) causing painful shoulder girdle movements on abduction and adduction
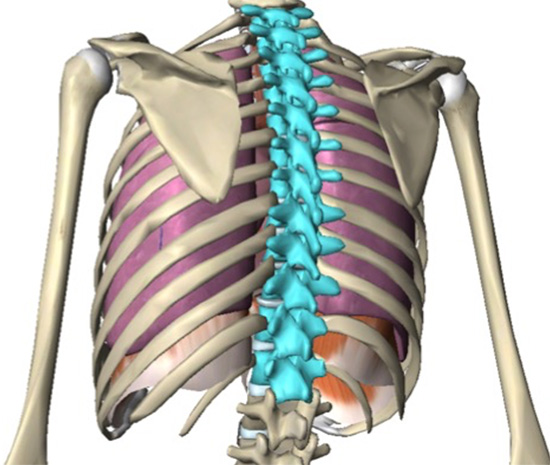
Thoracic Spine-rib complex
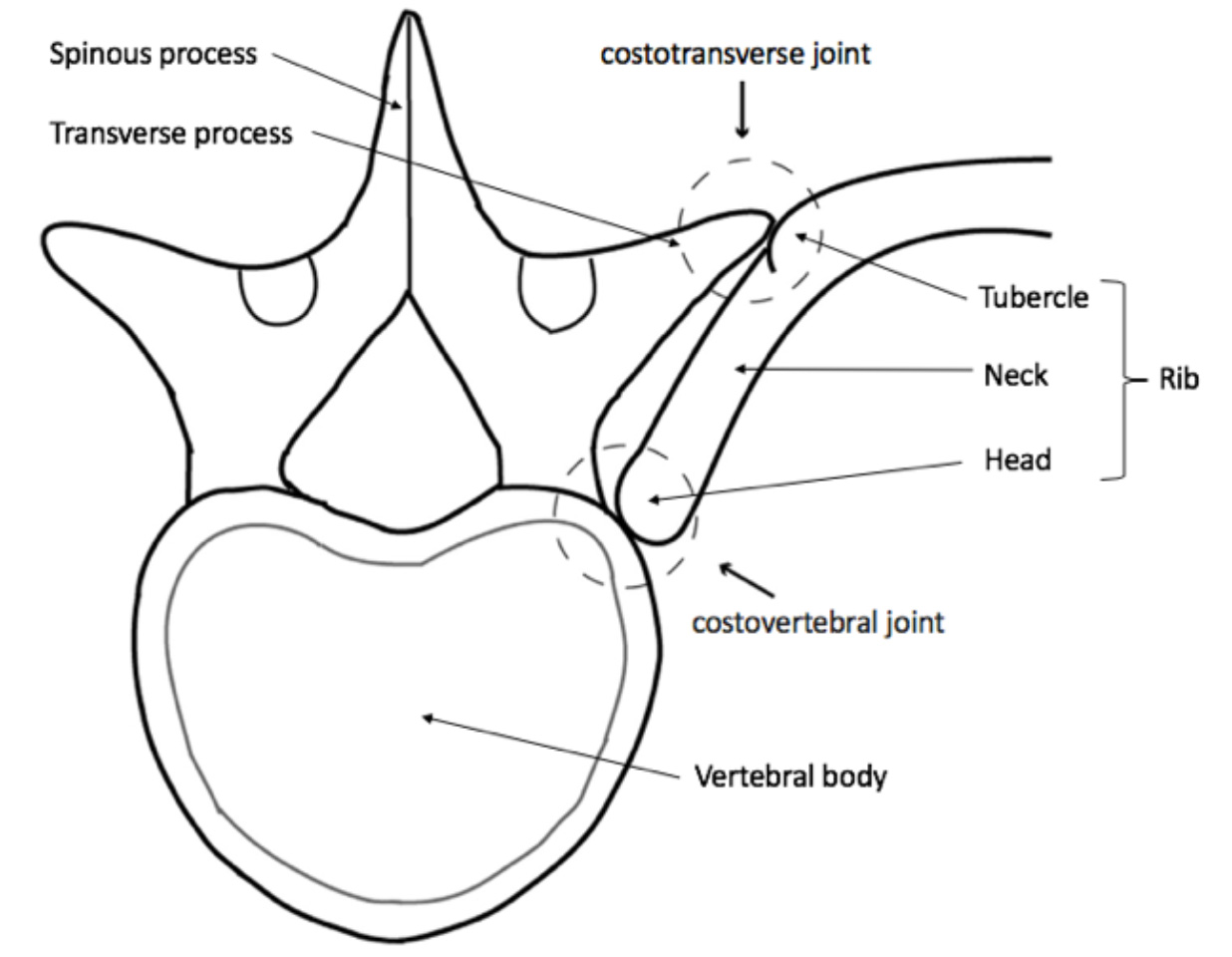
The Thoracic spine-rib complex refers to the spine or back between the 1st (level of the shoulders) and the 12th thoracic vertebra (bottom of the rib cage) and the 12 pairs of rib which attach to the vertebrae by the costovertebral and costotransverse joints. Each costovertebral joint (sometimes called costocorporeal joint) consists of 2 attachments or facets, the head of the rib articulating with the superior or upper costal facet of the corresponding vertebra, and the inferior facet that articulates with the head of the rib below. Only slight gliding movements can occur at these joints, due to the close articulation of their components. The costotransverse joint connects the tubercle of the rib (costal tubercle) with the transverse process of the thoracic vertebra. Each joint is surrounded by ligaments which support and stabilise the joints making movements of the ribs against the thoracic spine limited and specific (see buckle handle and pump handle movements).
Symptoms
Thoracic spinal problems can cause pain, typically a dull ache in the upper back that is made worse by deep breathing, coughing or rotation movements of the trunk and rib cage. The pain is often felt between the shoulder blades and to one side of the spine and may radiate around to the anterior chest wall. Other symptoms may include muscle spasm, a reduced range of movement particularly twisting or against resistance, stiffness and weakness.
| Causes of musculoskeletal thoracic spine pain | |
|---|---|
| Muscular inflammation – may be associated with: | Ankylosing spondylitis |
| • Poor Posture | Rheumatoid arthritis |
| • Spinal curvature (scoliosis, kyphosis) | Scheuermann's disease |
| • Minor muscle strain / trauma | T4 syndrome |
| • Repetitive overuse | Spinal stenosis |
| Joint dysfunction – may be associated with: | Diffuse idiopathic skeletal hyperostosis (DISH) |
| • Trauma / direct injury | Spinal tumours |
| • Osteoarthritis | Spinal infection (osteomyelitis) |
| • Inflammation | Vertebral body or rib fractures |
| Intervertebral ‘slipped’ disc protrusion or herniation | |
The most common cause of thoracic spinal pain is inflammation of the muscles or soft tissues of the thoracic spine and ribs. Muscular inflammation is most commonly caused by muscle irritation or tension, also called myofascial pain. The cause may be related poor posture (such as forward head posture) associated with skeletal conditions such as scoliosis and/or kyphosis or any type of irritation of the large back and shoulder muscles, including muscle strain or spasms associated with injury or over exertion, Sitting or standing in a slouched position over time, using a heavy backpack or repetitive activity.
Costotransverse and costovertebral joint dysfunction are disorders affecting or involving the joints and ligaments which can be overlooked during examination for pain source localisation. These joints can become painful in various ways. For example, cartilage tears and degeneration (osteoarthritis) can develop in the facet joints leading to inflammation, osteophyte formation and pain. In many cases, facet joint degeneration (osteoarthritis) and degenerative disc disease can happen at the same time. Other inflammatory conditions that can cause thoracic spinal pain include Ankylosing spondylitis.
Scheuermann's disease is a self-limiting skeletal disorder of childhood and describes a condition where the thoracic vertebrae grow unevenly resulting in the signature "wedging" shape of the vertebrae, causing kyphosis – an excessive outward curve of the spine resulting in an abnormal rounding of the upper back. The condition is sometimes known as "round back" or—in the case of a severe curve—as "hunchback." Another source of thoracic spine pain is T4 syndrome, when the T4 vertebrate and the joints surrounding this vertebra are injured or inflamed in some way leading to a specific set of symptoms including pain in the arm, headaches, neck pain and paraesthesia (numbness). It’s thought to be related to disruption of autonomic nerves.
It is also possible for a rib to become misaligned or displaced from the vertebrae either through injury, trauma or repetitive strain. In more severe cases, particularly in trauma, vertebrae or rib fractures can result. This may be associated with intercostal neuralgia (irritation of the intercostal nerve) and thoracic radiculopathy associated with compression on the nerve or nerve roots of the thoracic spine. When the symptoms radiate or refer distally from the spine into the back and outward along the ribs to the anterior chest wall it is considered radiculopathy.
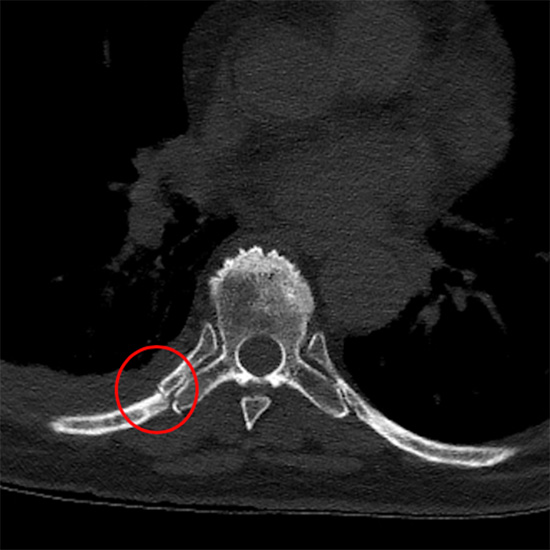
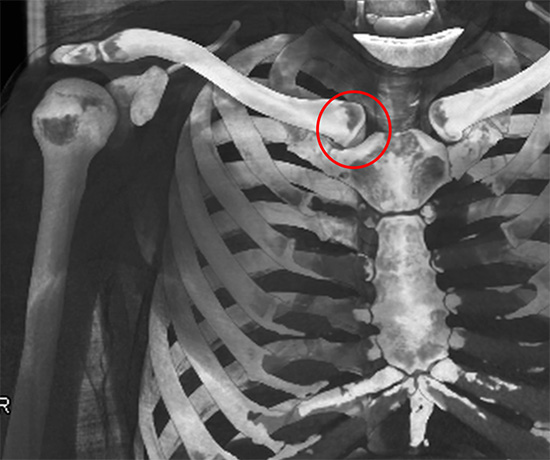
Chest CT following trauma showing rib fracture at neck of rib (red ring), note fracture through the adjacent transverse process
Non musculoskeletal causes of ‘visceral’ (or internal organs of the body) thoracic spine pain are important to exclude and may require specific tests. See also Non-chest wall related causes of chest pain.
Non musculoskeletal sources of ‘visceral’ thoracic spine pain
| Non musculoskeletal sources of ‘visceral’ thoracic spine pain | |
|---|---|
| Cancers | Including bone, lung, breast, kidney, pancreas |
| Cardiac conditions | Angina, myocardial infarction, pericarditis |
| Renal conditions | Kidney stones, kidney infection |
| Pulmonary conditions | Pneumonia, Pleurisy, Pulmonary embolism |
| Gastroesophageal conditions | Oesophagitis, gastritis, reflux |
| Gall bladder conditions | Gall stones, gall bladder infection |
| Hepatobiliary conditions | Hepatitis, pancreatitis |
Treatment
As with other chest wall problems such as chest wall pain or chest wall lumps treatment depends on the overlying cause. It may require further investigation to separate ‘local’, usually musculoskeletal causes such as shoulder or thoracic spinal MRI from visceral causes. For many types of Musculoskeletal causes, treatment options are similar. See Treatments.